
Mr Tanner has advised you to have macular hole surgery. This leaflet gives you information that will help you decide what to do. You may wish to discuss the information with a relative or carer. Before you have the operation, we will ask you to sign a consent form, so it is important that you understand the information in this leaflet.
The macula is a highly sensitive area of the retina that is used for fine vision and reading.
Unfortunately many diseases affecting the retina also affect the macula and can result in loss of vision. Macular holes are a relatively common cause of visual loss. The exact cause is still unknown, but macular holes are probably caused by the vitreous (the jelly-like substance inside the eye) pulling on the macula.
The macula is a highly sensitive area of the retina that is used for fine vision and reading.
The treatment involves surgery. Recent advances in the technology of micro-instruments and optical viewing systems now allow ophthalmic surgeons to perform surgery on the retina from within the eye. This has resulted in the successful treatment of complex eye problems, such as macular holes, which were previously untreatable.
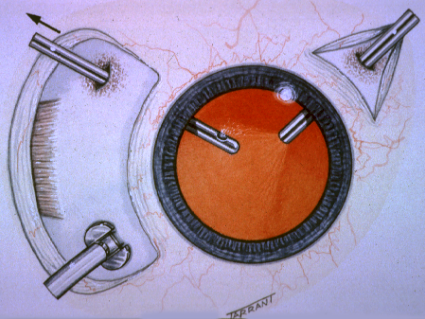
The treatment involves surgery. Recent advances in the technology of micro-instruments and optical viewing systems now allow ophthalmic surgeons to perform surgery on the retina from within the eye. This has resulted in the successful treatment of complex eye problems, such as macular holes, which were previously untreatable.
Mr Tanner now performs the majority of his macular hole surgery as a day case under local anaesthetic. General anaesthetic is still available for nervous patients. If having a general anaesthetic you should not eat or drink for 6 hours before the procedure. If having a local then light food and drink is allowed up to 1 hour before the procedure.
Before the operation both Mr Tanner’s team and the anaesthetist will speak to you and examine you on the ward. You will then be given eye drops to enlarge your pupils. When you arrive in the anaesthetic room a needle will be placed in your hand or arm.
During your operation three needle-sized holes are made in the white of the eye allowing removal of the vitreous jelly. This will allow Mr Tanner to repair the macular hole with delicate intraocular instruments which are used to remove any scar tissue holding the macular hole open.
The vitreous jelly will be replaced by a gas that will act as a support to hold the retina in position to help it to heal. Your normal body fluids will replace the gas naturally over 3-4 weeks.
Quite often Mr Tanner will remove mild cataracts as part of the same procedure.
Small stitches are usually placed in the eye and at the end of the operation we will put a pad or bandage over your eye to protect it and reduce swelling.
Following the operation we will usually ask you to keep your head in a face down position for 5 days. This is called ‘posturing’ and aims to provide support from the gas bubble to seal the macular hole. Posturing cushions will be provided and you should ensure that someone is at home to help you for the first 5 days. You only need to posture for 50 minutes every hour during the day and can sleep in your normal position.
Most studies have shown that posturing is not essential and if you have difficulties with adopting the correct position then it is possible to have a successful outcome, although closure rates are slightly lower
By following our instructions you will give your macula the best chance to be successfully treated. Your co-operation matters a great deal.
Because of the great difficulty in observing macular holes with conventional microscopic examination numerous high resolution imaging techniques have been introduced providing additional information on pathogenesis and prognosis. The most effective of these is Optical Coherence Tomography which uses low coherence interferometry to produce an optical cross section of the retina rather like an ultrasound image but with much higher resolution (10 um).
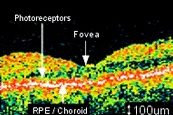
OCT of normal Macula
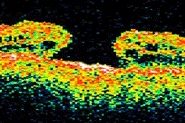
OCT of stage 4 Macula Hole (Vision 6/60 )
OCT of repaired Macula Hole (Vision 6/6 )
Most patients are able to leave hospital within a few hours of the procedure. If you have discomfort we suggest that you take a pain reliever, such as Paracetamol every 4-6 hours. It is normal to feel itching, sticky eyelids and mild discomfort for a while after macular hole surgery. It is common for your eye to water. Occasionally the area surrounding the eye can become bruised. Any discomfort should ease after 2-3 days. In most cases your eye will take about 6 weeks to heal. You will normally see Mr Tanner in the clinic 2 weeks after your operation. Try to rest while your eye is healing.
We will give you eye drops to reduce any inflammation and to prevent infection. We will explain how and when you should use them. Please do not rub your eye.
Certain symptoms could mean that you need prompt treatment. Please contact the hospital immediately if you have any of the following symptoms:
When you have a gas bubble in your eye you must not travel by aeroplane or ascend to significant altitude by other means of transport and must warn your doctor you have a gas bubble in the eye should you need another operation of any kind.
Mr Tanner’s most recent audit has confirmed a surgical success rate of 96% closure of macular holes and associated improvement in visual symptoms and reading ability. This data has been presented at national meetings and conferences. Mr Tanner has never had a case of serious intraocular infection following macular hole surgery.
Macular hole surgery is not always successful. Every patient is different. Around 5% of patients may need more than one operation.
There is a risk of complications, either during or after the operation. Minor complications are common and in most cases we can treat them effectively. Very rarely some complications can result in blindness.
Possible complications during the operation:
Possible complications after the operation:
If the first operation is not successful Mr Tanner will occasionally consider a repeat procedure, although this is not usually necessary.
Most patients undergoing macular hole surgery usually develop a cataract in the operated eye over the following 6 months. Cataract surgery is a much less invasive procedure and can be carried out as a day case under local anaesthetic. Occasionally Mr Tanner will combine the vitrectomy operation with cataract surgery.
If the first operation is not successful Mr Tanner will occasionally consider a repeat procedure, although this is not usually necessary.
Most patients undergoing macular hole surgery usually develop a cataract in the operated eye over the following 6 months. Cataract surgery is a much less invasive procedure and can be carried out as a day case under local anaesthetic. Occasionally Mr Tanner will combine the vitrectomy operation with cataract surgery.
Disclaimer : The information provided in this website is intended as a useful aid to general practitioners, optometrists and patients. It is impossible to diagnose and treat patients adequately without a thorough eye examination by a qualified ophthalmologist, optometrist or your general practitioner. Hopefully the information will be of use prior to and following a consultation which it supplements and does not replace.


